在2022年ASCO大会的前列腺癌教育专场(Education Session)中,加利福尼亚大学旧金山分校的核医学专家Thomas A. Hope教授带来了“Molecular-Based Imaging Redefining the Disease Landscape(分子成像重新定义疾病格局)”的主题报告。《肿瘤瞭望》在会议现场采访了Hope教授,分享他对前列腺癌分子成像及放射性配体疗法的看法。
编者按:在2022年ASCO大会的前列腺癌教育专场(Education Session)中,加利福尼亚大学旧金山分校的核医学专家Thomas A. Hope教授带来了“Molecular-Based Imaging Redefining the Disease Landscape(分子成像重新定义疾病格局)”的主题报告。《肿瘤瞭望》在会议现场采访了Hope教授,分享他对前列腺癌分子成像及放射性配体疗法的看法。
肿瘤瞭望
分子影像学技术与传统影像学方法有哪些区别?
Dr. Hope:成像通常涉及使用放射性标记小分子,比如镓(Ga)、氟(Fu)放射性物质,并且靶向于肿瘤细胞表面的分子标志物。分子影像学技术往往是功能成像,而常规成像技术通常是解剖成像。例如,CT或MRI只能显示器官的形态、大小等,而功能成像或分子成像可以显示肿瘤细胞表面的代谢或蛋白质表达。前列腺癌领域常用的骨骼扫描,实际上也是分子成像,在临床上已经应用很长时间了。
So molecular imaging typically involves labeling a small molecule with radio activity, right? So gallium, fluorine—something like that—and targeting a marker on a tumor cell surface. So, functional imaging, right? Conventional imaging, typically, is anatomic imaging. CT or MRI, you’re going to visualize an organ and seeing the physical dimensions of the metastasis. Whereas functional imaging or molecular imaging is going to show you a metabolic or a protein expression on the tumor cell surface. And it does get a little confusing in prostate cancer because a bone scan is actually molecular imaging, right? Because you’re looking at bone remodeling. But we bucket that into conventional imaging because it’s been around for so long.
肿瘤瞭望
除了像您提到的SPECT骨扫描,近年来前列腺癌领域还有哪些新型的分子影像技术或有潜力的靶点?
Dr. Hope:分子成像在前列腺癌领域取得了不少新突破,比如PSMA靶向放射性药物。目前FDA批准的DCFPyL、piflufolastat和PSMA-11等示踪剂药物,并已经成为美国的护理标准之一。从本质上讲,我认为所有这些放射性药物都是相同的,这是我们在一段时间内的发展方向。所以PSMA PET放射性药物不会很快出现下一代,但FDA批准这些药物不过一年半而已,我们还处在(PSMA PET靶向诊断和治疗)这个时代的开端。
So, in prostate cancer, I think we’ve come to, obviously, a new standing in molecular imaging, which is the PSMA targeted radiopharmaceutical—so PSMA PET. And that is sort of now at the FDA approval of DCFPyL and piflufolastat and PSMA-11. That’s now the standard of care in patients in the United States. And, in essence, I think of all those radiopharmaceuticals being identical, and that’s where we’re going to be for a while. So there’s not going to be sort of a next generation any time soon with PSMA PET radiopharmaceuticals. But that’s, you know, FDA approved a year and a half ago, so we’re at the very beginnings of that generation.
肿瘤瞭望
肿瘤细胞上表达的分子(比如PSMA)具有一定的异质性,这对诊断和治疗带来什么影响?
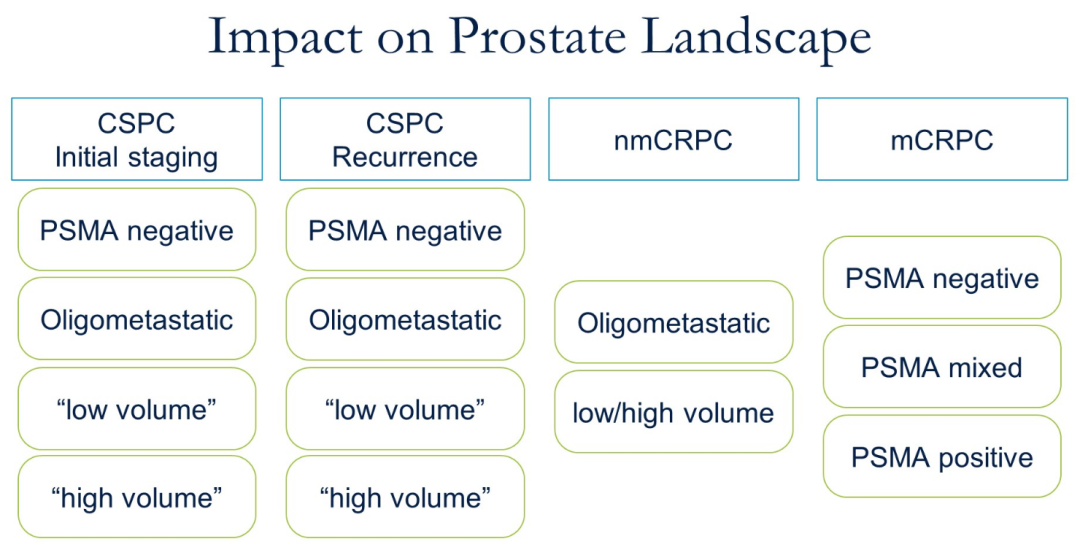
Dr. Hope:我会用两种不同的方式来看待异质性问题。对于更早期的患者,包括生化复发的患者或处于初始阶段的患者,其体内的肿瘤异质性水平很低。此类患者个体本身的肿瘤非常同质,但患者个体之间可能存在异质性。大约有5%的患者PSMA PET检查呈阴性,对于转移性疾病的敏感性非常有限。总的来说,当你查看PSMA PET阴性患者的文献时会发现,奇怪的是这些(早期PSMA阴性)患者表现非常好,是一个积极的预后因素。但对于去势抵抗性前列腺癌患者,当接受化疗、阿比特龙或恩扎卢胺治疗后肿瘤会表现出更强的异质性,这可能是一个非常糟糕的预后因素。在这种情况下,PSMA放射配体疗法往往不能覆盖所有的肿瘤病灶,FDG和PSMA摄取不一致的患者预后极差。因此,前列腺癌的异质性在不同疾病环境下是不一样。
So heterogeneity on PSMA PET. How does that impact prostate cancer? So I would think of them in two different ways. So if you think about patients’ earlier stage—so patients with biochemical recurrence or at an initial stage—and there’s actually very low levels of heterogeneity within a patient. So patients are typically very homogeneous within the individual patient, but there can be heterogeneity across patients. So maybe 5 percent of patients will be negative on a PSMA PET and that will have, obviously, a limited sensitivity forcing metastatic disease. Now, overall, when you look at the literature in patients who have negative PSMA PETs, those patients do very well so it’s a positive prognostic factor (oddly enough), even though you’re not seeing where the disease is, potentially. Now, in the castration resistance setting, when you’re after chemotherapy, after abiraterone or enzalutamide and you’re heterogeneous—that’s a very poor prognostic factor, right? And so PSMA radioligand therapy in that setting is not going to be very good at targeting the entire extent of disease. And so patients who have mismatched FDG and PSMA uptake have incredibly poor outcomes. So it’s very different depending on the setting of disease where you’re at.

肿瘤瞭望
未来,分子影像学技术在前列腺癌领域将有哪些研究方向?
Dr. Hope:展望放射药物和PSMA成像方面,我还看不到太多,因为很多临床试验正在进行中。目前有涉及rhPSMA-7、18F-PSMA-1007的三期研究,未来几年将有更多的PET放射性药物获得FDA批准。这些药物在功能上与PSMA-11和DCFPyL几乎相同。目前正在改变的是前列腺癌的治疗现状。我们可以看到Lu-PSMA-617在3月份获得FDA批准。这显然将对mCRPC患者产生巨大影响。我们现在还有PSMA4、SPLASH、ECLIPSE等III期随机试验正在进行中,以及先进行预化疗再序贯PSMA放射性配体疗法的研究。但我认为更令人兴奋的是改变不同配体中的放射性核素。例如,使用锕(Ac)或铅(Pb)等α线发射器有助于提高PSMA放射性药物的疗效。因此,我认为在未来几年,大部分的发展将是在治疗方面,而不是在成像方面。
So looking forward with radiopharmaceuticals and PSMA—so on the imaging side, I don’t see much. What I mean by that is there are obviously a lot of clinical trials going on. There are phase III studies involving rhPSMA-7, 18F-PSMA-1007—so there will be more PET radiopharmaceuticals that will be FDA approved in the coming years, but it’s not going to change the needle. Those are pretty much functionally identical to PSMA-11 and DCFPyL. Now, the thing that’s going to change things in prostate cancer is on the therapy side, right? So we just saw approval of Lu-PSMA-617 in March, right? By the FDA. And that’s obviously going to be hugely impactful for men who have castration resistant prostate cancer. And then you have the PSMA4 SPLASH ECLIPSE Phase III randomized trials and prechemotherapy—so slowly moving up PSMA radioligand therapy. But I think the thing that’s more exciting there is changing radionuclides in different ligands right? So using alpha emitters like actinium or lead to help increase the efficacy of PSMA radiopharmaceuticals moving forward. So, most of the development is going to be on the therapeutic side rather than on the imaging side, I would think, in the coming years.
Thomas A. Hope, MD
加利福尼亚大学旧金山分校核医学专家
服务于加利福尼亚大学旧金山分校医疗中心、旧金山退伍军人事务医疗中心等多所医院。他于斯坦福大学医学院获得了医学博士学位后,在核医学领域工作近20年,多项研究成果发表于JAMA Oncol、Lancet Oncol、Clin Cancer Res等国际期刊。





 京公网安备 11010502033352号
京公网安备 11010502033352号